Unwinding of PHE for Medicaid in Missouri: February Update
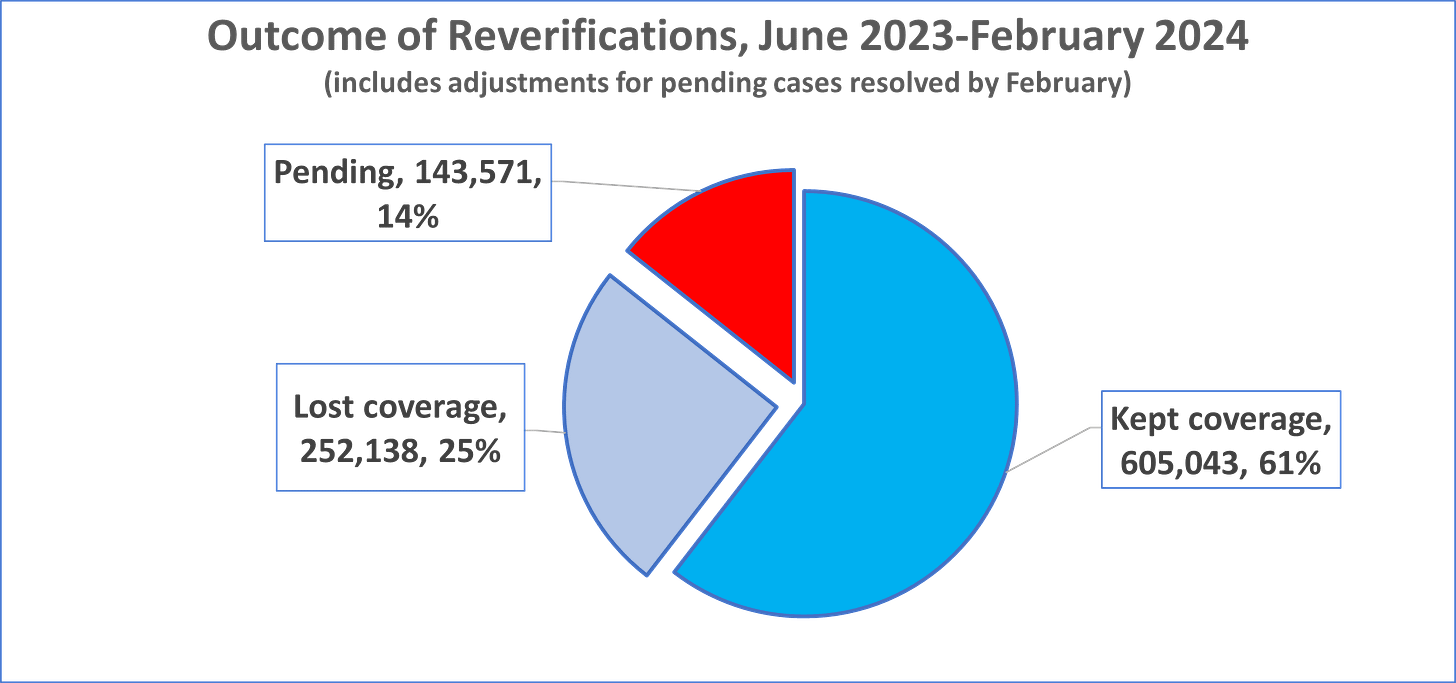
Missouri has reviewed over one million eligibles in nine months. Over 605,000 retained coverage, but over 250,000 have lost coverage, including over 119,000 children. Over 140,000 cases are pending.
UPDATE FOR FEBRUARY 2024.
The first nine months of data have now been reported by the state of Missouri in a public dashboard. This post reviews some of the major conclusions from this data, computed by this author from the state’s dashboard.
Nationwide Medicaid enrollment rose to a record high during the pandemic, and in Missouri the enrollment also rose to over 1.5 million, a record.
According to analysis by the Center for Advancing Health Services Policy and Economics Research at Washington University in St. Louis, the State of Missouri has reviewed over one million recipients from June 2023 to February 2024. Over 605,000 have retained coverage, but over 250,000 have lost coverage, including over 119,200 children. Over 143,000 cases remain pending.
The numbers for Missouri can be compared to other states using, for example, the Kaiser Family Foundation’s unwinding website, which is being continuously updated. Over 19 million Medicaid enrollees have been disenrolled and over 40 million have had their coverage renewed, as of March 26, 2024.
Some major points about Missouri’s unwinding:
From June 2023 to February 2024, slighly more than one million (1,000,762) Medicaid cases have been reviewed in Missouri. The state’s plan is to review the total set of enrollees over a 12-month period.
Over the nine months, 61% (605,053) of recipients have been determined still eligible for Medicaid, while 25% (252,138) have lost coverage (been declared ineligible or lost coverage through a procedural determination). Another 143,571 (15%) are pending review.
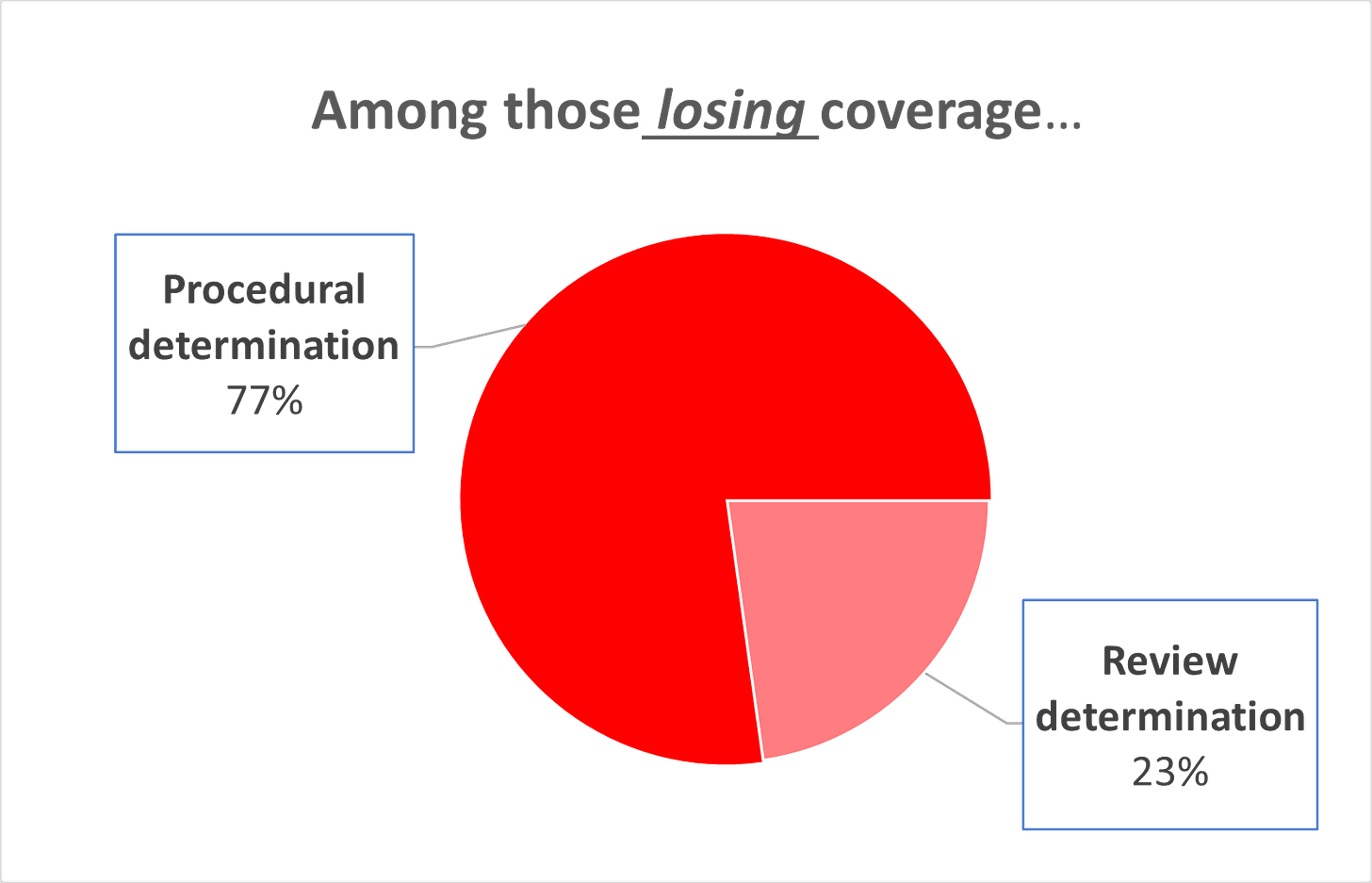
Of those losing coverage over the nine months, 77% lost coverage for a “procedural determination” according to the state, which can be due to a range of reasons, while 23% lost coverage because they were reviewed and determined no longer eligible for the program. High “procedural determinations” is a metric being used widely to measure how states are doing (see Kaiser’s analysis) with their Medicaid redeterminations.
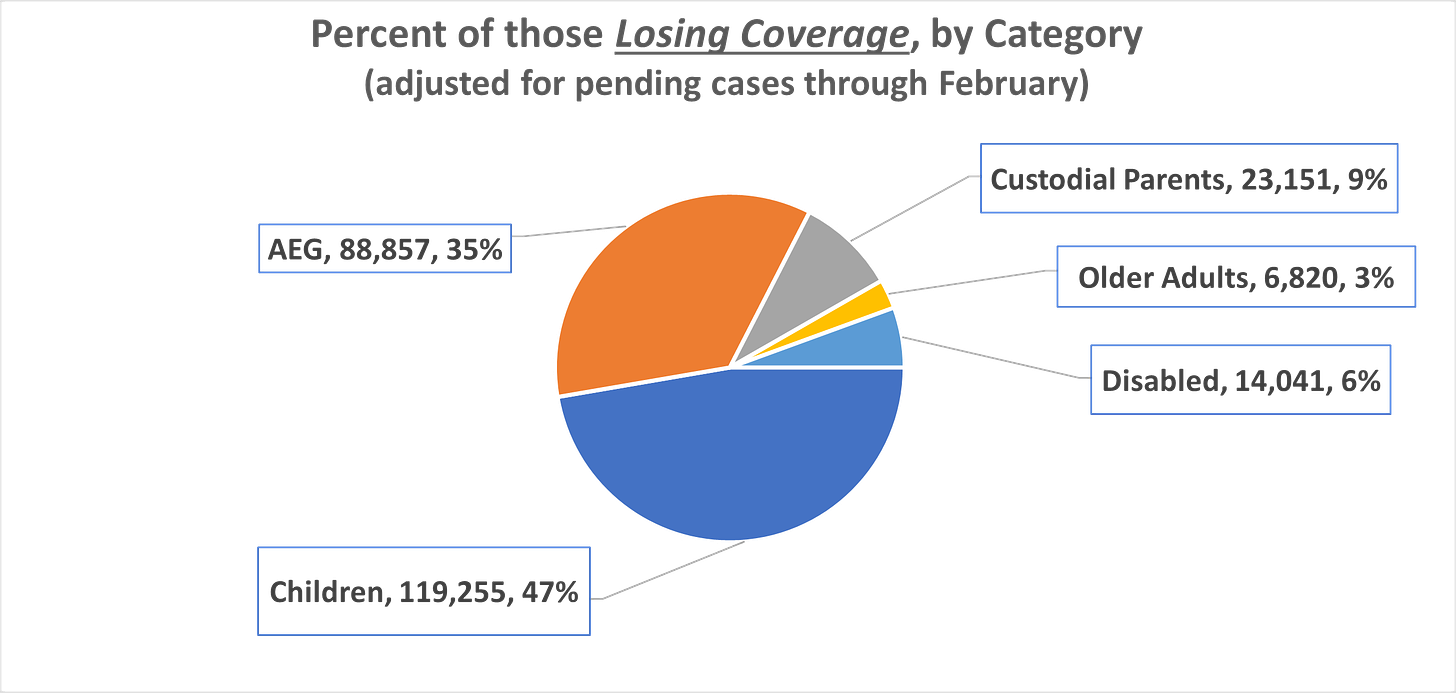
Of the total persons losing coverage so far over nine months, 47% (119,255) were children, 35% (88,857) were expansion adults, with the rest in other categories (see chart).
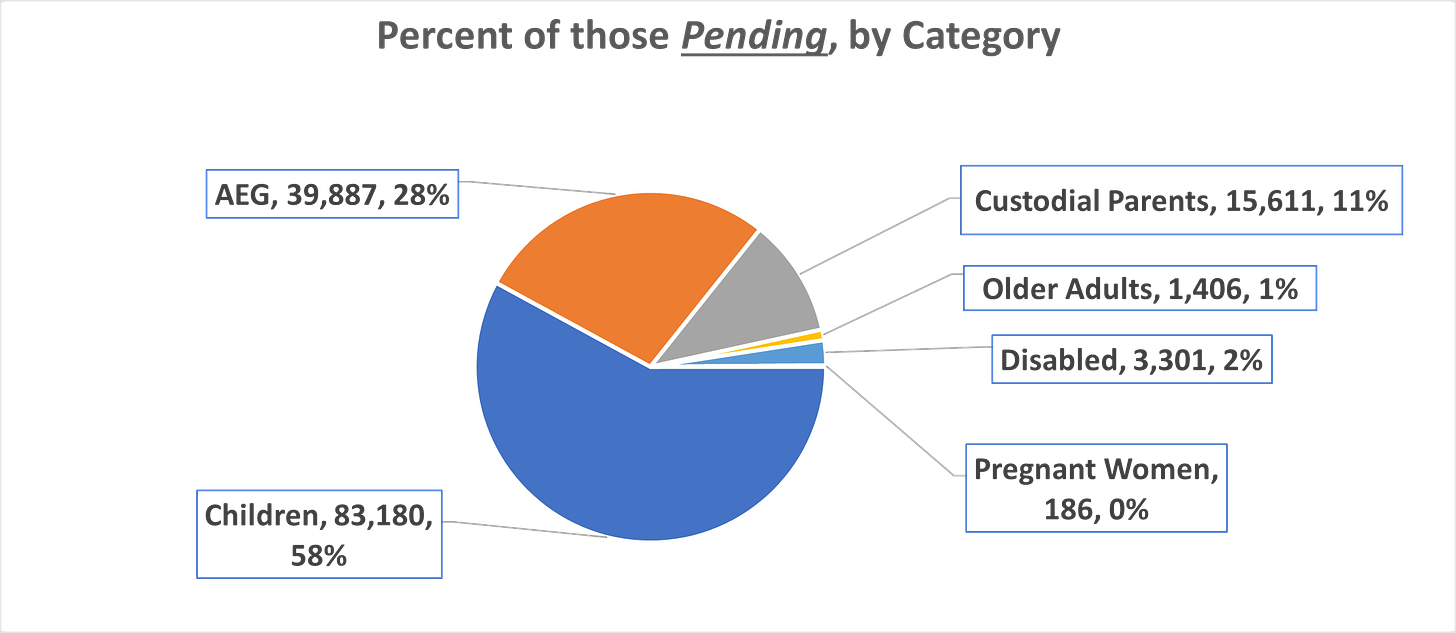
At the end of nine months, over 143,000 cases remained pending (an increase over the the 133,000 pending at the end of January 2024). Of the pending cases, 58% of the pending applications were children and 28% were expansion adults, 11% were custodial parents with the rest being in other categories (see Chart).
The process of recertifying enrollment in Medicaid, which generally had been done on an annual basis before the COVID pandemic, was paused during the Public Health Emergency (PHE) by federal law in early 2020. This meant that those enrolled in Medicaid during that period were not disenrolled. Federal law passed at the end of 2022 called for an end to the PHE, and a renewal of the recertification process, commonly called the “unwinding” of the pandemic as it is affecting Medicaid. The state also reported these data by law to the Centers for Medicare and Medicaid Services (CMS).