December 2024 Update: Missouri Medicaid six-months of reverifications completed
Medicaid enrollment has remained steady in last six months. However enrollment has grown in the Adult Expansion Group, offsetting drops in other categories
January 13, 2025 (updates based on December 2025 state administrative data).
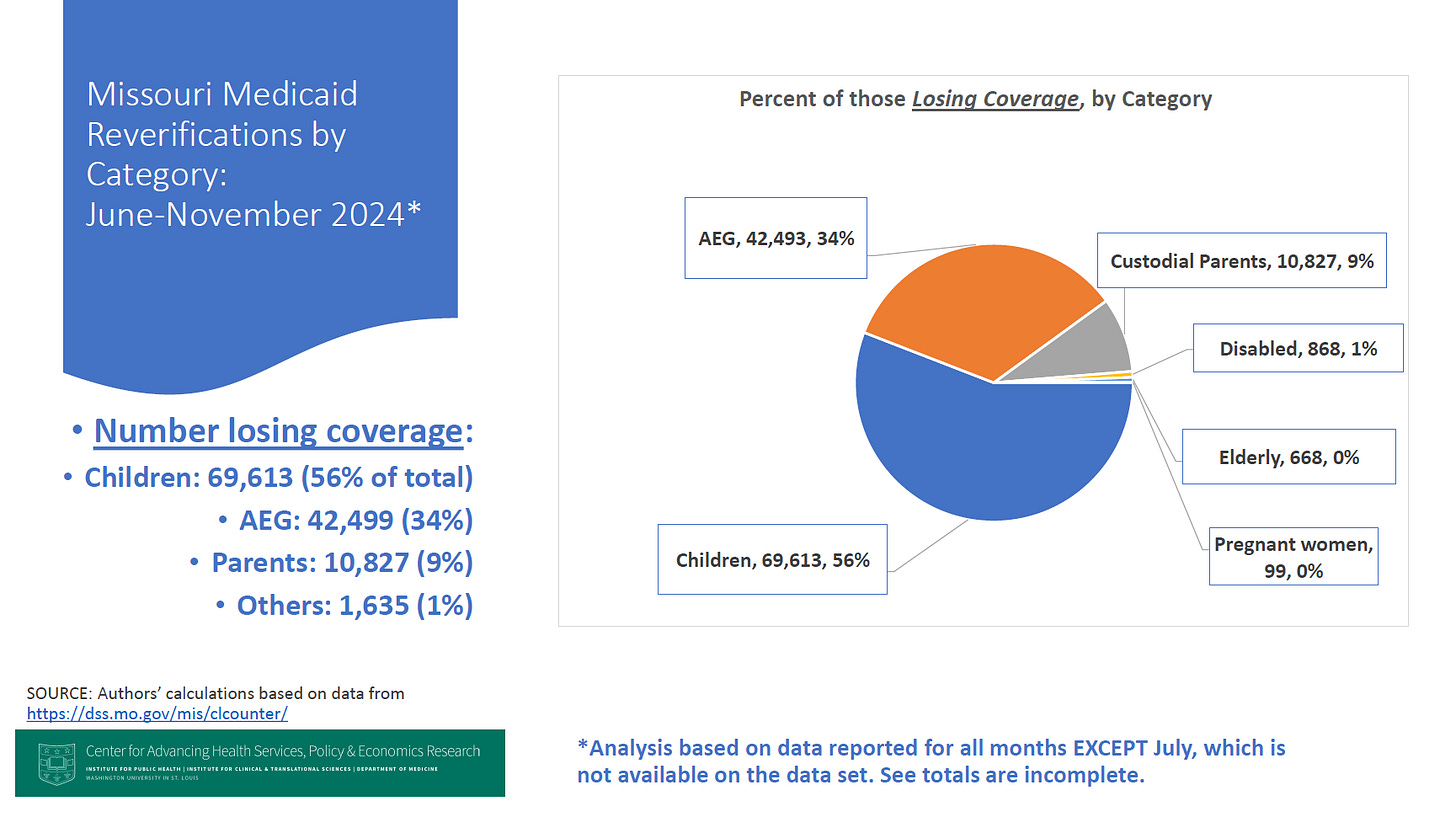
Since the Public Health Emergency (PHE) ended in Missouri and across the U.S. in May 2024, the state began regular reverications of annual enrollment for persons on MOHealthNET (Medicaid). Since that time, the state of Missouri has reviewed over 540,000 cases in the six months from June through November of 2024. Most recipients have retained their coverage (57%) but about one-quarter (27%) have lost coverage in this process, with 16% cases still pending. During this period, total net enrollment in Missouri’s Medicaid program has remained relatively flat at about 1.27 million in November. However, since May 2024 there has been significant drops in enrollment in several categories — especially children, custodial parents, and the disabled — but these drops have been offset by increases in enrollment in the Adult Expansion Group (AEG).
These findings are based on analysis by CAHSPER at Washington University in St. Louis of state of Missouri Family Support Division data, posted on their website.
Factors affecting enrollment. The changes in enrollment may reflect changes in the process of reverifying enrollment (a regular process done annually), as well as normal growth in Medicaid over time due to population growth. During the Public Health Emergency (PHE) annual reverifications of Medicaid enrollment were paused by the federal government, which meant that those enrolled in Medicaid during that period were not disenrolled. Nationwide Medicaid enrollment rose to a record high during the pandemic, and in Missouri the enrollment also rose to over 1.5 million, a record. Federal law passed at the end of 2022 called for an end to the PHE, and a renewal of the recertification process, commonly called the “unwinding” of the pandemic as it is affecting Medicaid. The process of recertifying enrollment in Medicaid began again in June 2024, which generally had been done on an annual basis before the COVID pandemic, after the unwinding process ended in May 2024. Missouri residents continue to enroll in Medicaid through the expansion, or through other categories, or re-enrolled after losing their coverage (called churning). Thus the numbers reported here show the net effects of the unwinding plus new enrollees.
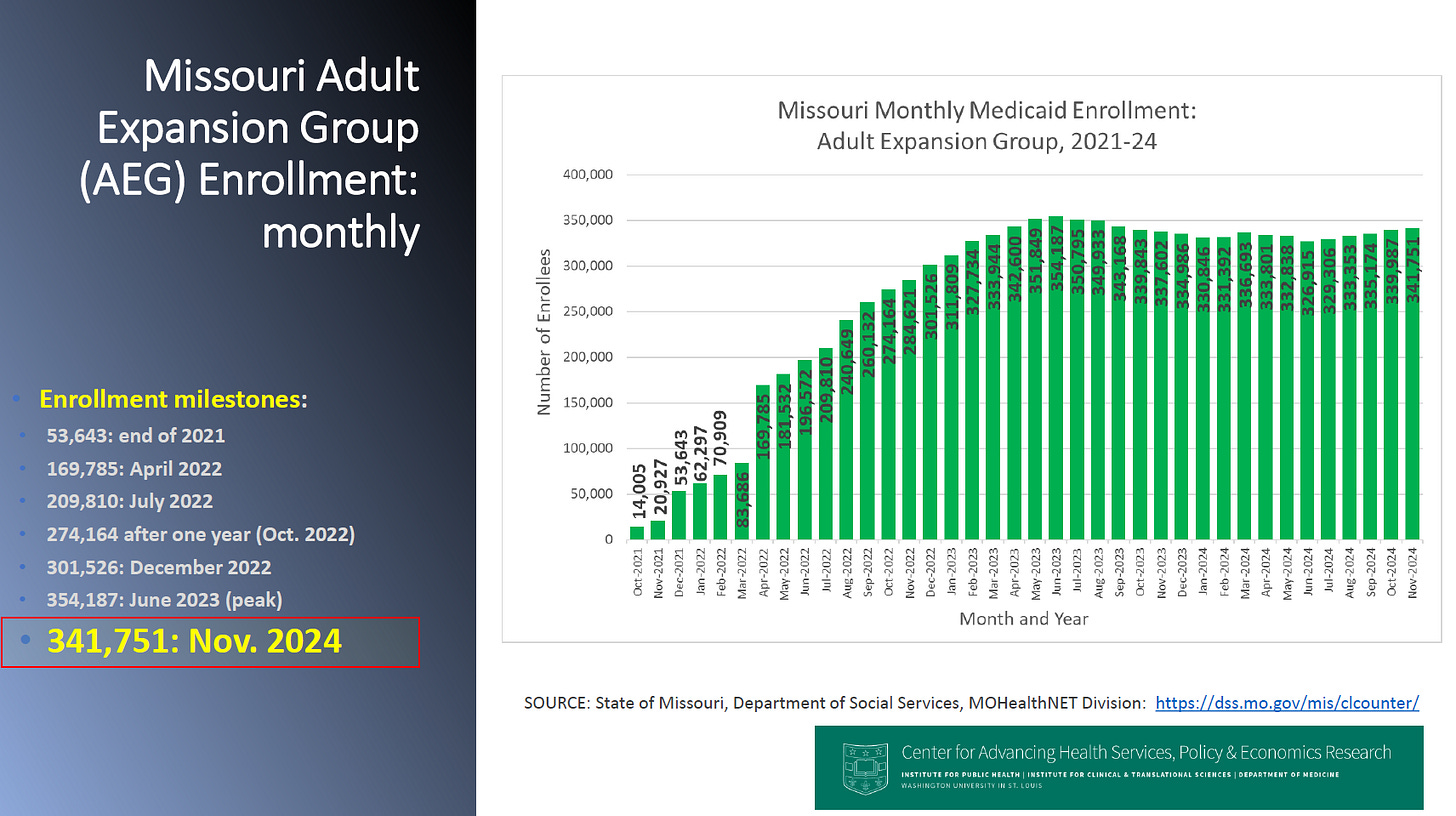
Enrollment growth led by Adult Expansion Group (AEG). As noted, net enrollment in Missouri’s Medicaid program has increased slightly to 1.271 million in November 2024, from 1.267 million in June 2024. The growth in enrollment is being driven though by a rise of 8,913 in the Adult Expansion Group (AEG) since May 2024. Growth also occurred in the pregnant women category and Women’s Health Services Program (up over 6,000 over that period, not shown in the figure). This has been offset by drops in enrollment in other categories — children, persons with disabilities, custodial parents — since May 2024. The changes may suggest that some people who are losing Medicaid coverage through the reverifications are signing up through the AEG, or that there are new enrollees replacing that lost coverage.
Update on Medicaid expansion. As noted, the expansion of Medicaid began in Missouri in July 2021, with the first people enrolled in October 2021. As shown in the graph, the current enrollment in the Adult Expansion Group (AEG) is 341,751 in November 2024. AEG enrollment fell in the first seven months of the unwinding, but has grown over 14,000 in recent months, perhaps suggesting there is some churning from other categories into the AEG from other populations.
2024-25 Annual Reverifications. The first six months of data on reverifications have now been reported by the state of Missouri in a public dashboard, and also reported by law to the Centers for Medicare and Medicaid Services (CMS). Although that dashboard reports the data nicely in graphics, a summary of the data is not provided. Here a summary of the outcome of the total reverications over the six months is reported. In addition, the state is not reporting data on reverifications for July 2024, though that data has been reported to CMS and that data is used here.
Some major points:
Pver six months (June to November 2024), about 542,000 Medicaid recipients have been reviewed (see graph). The state’s plan is to review the total set of enrollees over a 12-month period.
Over the first six months, 57% of those reviewed have been determined still eligible for Medicaid, while 27% have been declared ineligible or lost coverage. Another 16% are pending review.
Of the recipients who were declared still eligible for coverage, 52% were approved by “ex parte” (the state’s records demonstrated that they were still eligible), and 5% were declared eligible by application to the state.
Of those losing coverage, over the first two months, 91% lost coverage for procedural reasons as opposed to 9% being declared ineligible for coverage based on a review of the prepopulated form submitted.
Of the total persons losing coverage over the first two months, slightly more than half are children (56%), 34% are from the adult expansion group, 9% are custodial parents, with a small number in the other categories — disabled, elderly, and pregnant women. These findings are based on some incomplete information since the state has not reprted data for July 2024.
__________
Report prepared by analysts at Center for Advancing Health Services Policy and Economics Research (CAHSPER), Institute for Public Health (IPH), Washington University in St. Louis.